|
|
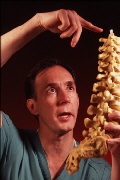
"Based on my experience," says James
Campbell, "opiods are more effective than any single class
of drugs for pain relief."
|
|
But Campbell and several other Hopkins specialists who prescribe
opioids for chronic pain often run up against obstacles. They say
that many doctors who are afraid to prescribe the drugs are
clinging to outdated conventions--such as the belief that opioids
inevitably cause addiction or intolerable side effects. Others
who do see the benefits of opioid medications still avoid
prescribing them because they fear that state medical boards will
take away their licenses, as has occurred recently in a handful
of high-profile cases.
"Opioids are among the most stigmatized medicines," says
neurologist Russell Portenoy, chairman of pain medicine and
palliative care at Beth Israel Medical Center in New York and
president of the American Pain Society. "There is an enormous
number of myths and misconceptions that physicians and the public
perceive."
As a consequence, Campbell and several other Hopkins pain
specialists now routinely spend time talking with referring
physicians to correct mistaken notions and explain the state of
the art for using opioids for chronic pain.
"We're trying to mount education for the [medical] community at
large. A lot of education is needed in the primary care setting,"
says Nathan Rudin, an assistant professor of physical medicine
and rehabilitation. "Physicians need to know that if these
medications are used properly, prescribing them is as routine as
prescribing a blood pressure medicine. It doesn't need to carry
any more of a stigma."
BUT CAMPBELL AND COLLEAGUES face an uphill battle, as Patricia
Townson's case demonstrates.
After her car accidents, Townson tried chiropracty, electrical
stimulation, and a large variety of medications, all futile
attempts to relieve her pain. Finally, a pain specialist
prescribed morphine. While no cure, the pills gave her enough
relief that she was able to visit friends for an hour.
Her troubles continued this past January, however, when she had
surgery to remove two disks in her neck. Her surgeon, says
Townson, was horrified to find that she was taking morphine, and
he forbid her to continue its use. Townson complied with his
recommendation, but after a few days her pain was unbearable.
Her husband rushed her to the emergency room in the middle of the
night, as she writhed in agony; her misery was no doubt
compounded by the effects of morphine withdrawal. "My body was
drenched. My clothes were drenched. The pain in my neck was just
so severe. I just wanted to die," she recalls today.
Townson's doctors told the ER staff that she should be placed in
detox, but the detox program refused to admit her. So she was
sent home.
In February, Townson's husband rented a van, made a bed for his
wife in the back, and drove her to James Campbell's office at
Hopkins. After examining Townson and studying her medical
records, Campbell recommended that she continue taking the
morphine medication. He also wrote a letter to her local
physician explaining the merits and safe use of the drug.
Townson's physician grudgingly agreed to give her a two-month
supply of the drugs with the idea that she would gradually wean
herself off of it. The dozen other doctors she's tried calling
have refused to write her a prescription for the medication. "So
I'm blackballed," she says.
Townson is not alone in her pain. According to the National
Institute of Neurological Disorders and Stroke, 40 million
Americans each year visit a doctor for chronic pain. Headache and
back pain top the list of chronic pain conditions. Others include
arthritis, endometriosis, temporomandibular joint pain (TMJ),
vulvar pain, trigeminal neuralgia, shingles pain, and
fibromyalgia. (Cancer patients, of course, also experience
chronic pain, and have had to wage their own battle for adequate
pain relief. However, the question of using opioids for
non-malignant chronic pain is a more recent controversy.)
Deciding when pain should be described as chronic is somewhat
arbitrary, says Campbell. By and large, patients who rate their
pain as a seven or above on a zero-to-10 scale, and whose pain
has lasted four to six weeks or more,"start verging on chronic,"
he says.
But chronic pain patients present notoriously complex cases
because their injury or disease is often compounded by other
problems, such as depression and physical disability. Physicians
often have a difficult time untangling the web of ailments that
can occur with chronic pain. Such pain can endure for a decade or
more, and it is not uncommon for patients to seek the help of
dozens of doctors, depleting their savings in the process--a pain
treatment odyssey that some physicians mistake for the "doctor
shopping" of a drug abuser. A recent survey by the American Pain
Society, the American Academy of Pain Medicine, and Janssen
Pharmaceutica concludes that more than 40 percent of people with
chronic pain are not receiving adequate pain relief.
Many of the patients who cannot find or are denied adequate pain
control are angry, bitter, and desperate. The tenor of the
messages posted electronically on the listserver maintained by a
patient support and advocacy group called the American Society
for Action on Pain (ASAP) reflects this range of sentiments.
Some patients write that their doctors allot them only one
short-acting opioid pill per day. The medication lasts only four
hours, leaving them in pain for the other 20 hours.
Other patients were taking methadone, for pain, but were taken
off the drug "cold turkey" because hospital staff said they were
addicted to the medication. Several patients posted messages in
recent months requesting the address of Jack Kevorkian, or
debating the ethics of physician-assisted suicide.
ASAP's founder, Skip Baker, has lived with chronic pain for 20
years. A photographer based in Williamsburg, Virginia, Baker has
a rare disease called ankylosing spondylitis. For years, he
looked for a physician who could alleviate his pain. He even
bought a shotgun and contemplated suicide. Finally, a doctor
diagnosed his condition and put him on morphine. Now almost
entirely pain-free, he is trying to help other patients. "My
hobby," he says, "seems to have become getting severe chronic
pain patients to doctors willing to control their suffering
rather than letting them go to Dr. Kevorkian or take their own
lives."
Baker has also written letters to and testified before state
medical boards, and helped organize a march on the Capitol by
pain patients to demand better pain management. Many doctors, he
says, "are terrified to treat pain for fear of getting
prosecuted." He maintains a "barbaric list" of states where
patients have reported the most egregious pain management
practices. Many medical boards, says Baker, "assume we're taking
pills to get high."
|